Understanding The 5-Star Ratings And Quality Measures
Di: Everly
Understanding Measures, Star Ratings, and Quality Outcomes October 11, 2018 2:00-3:00 P.M. ET. Agenda Topic Speaker Dialysis Facility Compare: Review and Background Elena K.
Understanding these Two HEDIS Measures Two additional HEDIS measures are now included for health plans’ Star Ratings scoring: Transitions of Care and Follow-up after ED Visit for People
Understanding the Medicare Star Quality Ratings
Star Ratings support providers to understand their performance and drive improvement using nationally consistent measures to monitor, compare and improve their care. Star Ratings are
To learn more about MA Star Ratings, check out our article Understanding Medicare Advantage Star Ratings: What They Mean For Providers And Patients.. Why CMS Raised the 2025 Stars
Tips for Using Star Ratings When Choosing a Plan. Look for High Ratings: Plans with 4 or 5 stars generally provide better quality and value. Compare Benefits: Use star ratings
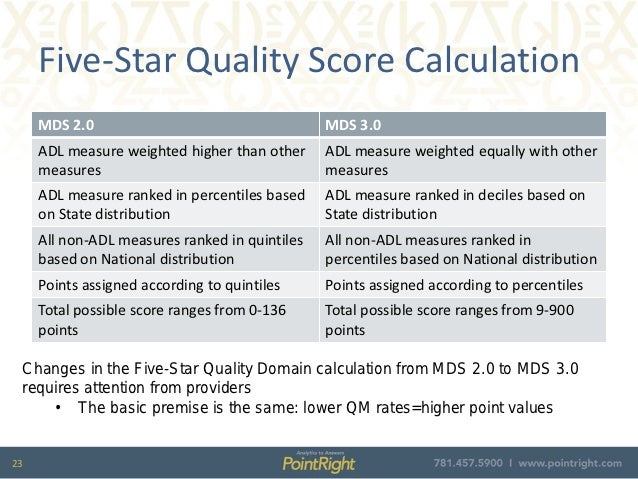
The Five-Star Rating looks at three components: onsite health inspections or surveys by the state, Quality Measures derived from the MDS assessment, and staffing levels either reported on the 671/672 reports or
- What Are Medicare Plan Star Ratings and How Are They Measured?
- A Guide to the CMS Nursing Home Quality Star Rating
- Understanding the 5-Star Ratings and Quality Measures
Multiple studies show evidence of a strong correlation between nursing home staffing levels and quality of care.[i] Federal law requires sufficient staffing levels to safely meet
CMS developed the DFC Star Rating to help patients, caregivers, and other healthcare consumers understand CMS quality measures and more easily identify differences in overall
Understanding Medicare’s 5-star rating hospital program
The CMS 5-Star Ratings are simple and user-friendly for patients, but understanding exactly how the ratings are calculated can be complicated from the perspective of a nurse leader.
Understanding the Medicare Star Quality Ratings 2025. Providing detailed information on the Medicare Part D prescription drug and Medicare Advantage plans for every state, including
The most recent refresh reflects the inclusion of these four previously paused measures. In reviewing the data and preparing for the quarterly release, CMS lowered the
Learn how to improve your nursing home’s 5-star rating by focusing on key quality measures like hospitalizations, antipsychotic use, and pressure ulcer prevention. Practical tips
MDS 3.0 QM User’s Manual V16.0 (MDS-3.0-QM-USERS-MANUAL-v16.pdf) contains detailed specifications for the MDS 3.0 quality measures, as well as the Quality
- 7 Key Insights on 5 Star Rating CMS for Healthcare Success
- CMS 5 Star Rating; Quality Measures
- 5-Star Staffing Rating Simplified
- Five-Star Refresh: A Look at Quality Measures
Understanding Measures, Star Ratings, and Quality Outcomes October 11, 2018 2:00-3:00 P.M. ET. Agenda Topic Speaker Dialysis Facility Compare: Review and Background Elena K.
Understanding Measures, Star Ratings, and Quality Outcomes June 29th, 2023. Agenda 6/29/23 3 Agenda Topic Speaker October 2023 Release Overview Golden Horton, MS Technical Lead,
Nursing homes with 5 stars are considered to have much above average quality and nursing homes with 1 star are considered to have quality much below average. There is
So, what is a Star Rating? Medicare uses a five-star quality rating system to evaluate health plans. The Star Rating can tell you a lot about a company’s customer service, member
Understanding Measures, Star Ratings, and Quality Outcomes January 23, 2020 12:00pm ET . Agenda Topic Speaker Dialysis Facility Compare: Review and Background Golden Horton, MS
Medicare star ratings are an objective measure for you to compare private Medicare Advantage and Medicare Part D plans based on the quality of care and performance.
• Add one star to Step 2 if quality measure rating is five stars. • Subtract one star if quality measure rating is one star. • The overall rating cannot be more than five stars or less than one
The Centers for Medicare & Medicaid Services (CMS) developed the 5-Star Quality Rating System to help consumers, families, and caregivers compare nursing homes more easily.
Under this program, CMS withholds 2% of Medicare Fee-for-Service (FFS) payments annually and pays a portion of that amount back based upon performance on preventing hospital
The Nursing Home Five-Star Quality Rating System is a program developed and maintained by the Centers for Medicare and Medicaid Services (CMS) to evaluate and
Things are slightly different with the above Short Stay measure. Notice the point values in parentheses? Since there are fewer Short Stay measures than Long Stay, the Short Stay
CMS Five-Star Quality Rating System: Importance and Impact on Healthcare Facilities. The 5 star rating cms serves as a vital resource for consumers evaluating the quality
How are CMS star ratings determined? The ratings include specific clinical, member perception and operational measures. There are approximately 40 measures in the star rating framework.
< Quality measure specifications are available in the QM Users’ Manual download file, which can be found under the Downloads section below. A sub-group of quality measures
Understanding Measures, Star Ratings, and Quality Outcomes June 20, 2018 1:00-2:00 P.M. ET. Agenda Topic Speaker Dialysis Facility Compare: Review and Background
The 5-Star Rating System Provides consumers with Overall Quality Rating of one to five stars based on performance for three types of measures, each with its own five-star rating: Health
Add one star if the Quality Measure rating is 5 stars; subtract one star if the Quality Measure is 1 star. The rating cannot go above 5 stars or lower than 1 star.
The Five-Star Quality Rating system is comprised of three parts, referred to as domains: health inspections (survey), quality measures and staffing. A rating of one to five stars is given to each of the three domains, which are combined
- Myanimelist Top 100 Anime – Lista De Animes
- Campinghammer Mit Auszieher – Campinghammer Testsieger 2021
- Mitsubishi Outlander: Bremsen Wechseln
- Immobilien In Der Region Kühlungsborn
- Zoll Korea _ Zollbestimmungen Südkorea
- Senate Passes Historic Native American Health Legislation
- Where Is My Taskbar? _ My Taskbar Is Missing
- Stranger Things Season 4: Everything To Know
- Melatonin Alter _ Melatonin Schlafen
- Die Einsamen Wölfe: Einsamer Wolf Persönlichkeit
- Studienkreis Nachhilfe München-Trudering
- Museum Fünf Kontinente In München: Kulturen Aus Aller Welt
- Clean Energy Bill Passes, Byron Nuclear Power Plant Saved