Risk Of Upper Gastrointestinal Bleeding In Patients On Oral
Di: Everly
Acute upper gastrointestinal bleeding in patients on long term oral anticoagulation therapy: endoscopic findings, clinical management and outcome . World Journal of
Management of Nonvariceal Upper Gastrointestinal Bleeding
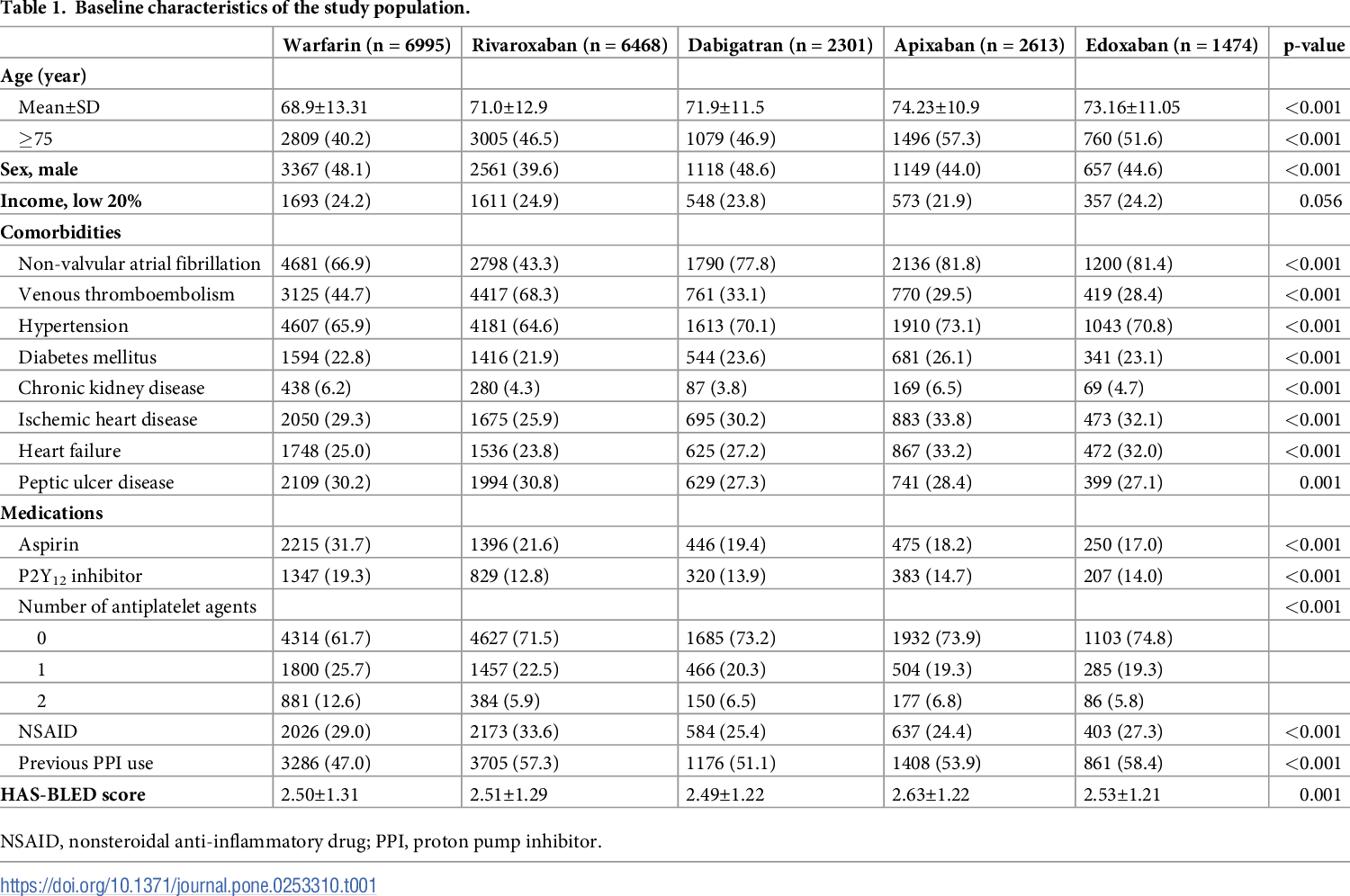
Objective To evaluate if proton pump inhibitor (PPI) treatment reduces the risk of upper gastrointestinal bleeding (UGIB) in patients with atrial fibrillation (AF) treated with non-vitamin K
In patients with atrial fibrillation (AF) receiving direct oral anticoagulant (DOAC), upper gastrointestinal bleeding (UGIB) is a serious complication. There are limited data on the benefit of preventive proton pump inhibitor (PPI) use to reduce the
Narrative Upper gastrointestinal bleeding (UGIB) is common, with an annual incidence of approximately 67 to 150 per 100,000, with estimated mortality rates between 6% and 15%.1
- Association Between Oral Anticoagulant PPI Cotherapy and UGl Bleeding
- Non-vitamin K antagonist oral anticoagulants, proton pump
- Proton Pump Inhibitors for Acute Upper Gastrointestinal Bleeding
Here, we examine current evidence linked to GIB associated with oral anticoagulants, with a focus on randomized control trials, meta-analyses, and postmarketing observational studies. Rivaroxaban and dabigatran (especially
Therapy, and the Risk of Gastrointestinal Bleeding D ual antiplatelet therapy (DAPT) with aspirin and oral P2Y 12 in-hibitors remains the cornerstone of therapy for patients with acute coronary
The results suggest that DOACs may be preferable to warfarin in patients with a history of peptic ulcer disease or major upper GIB. However, there are a few issues with the study that need to
Risk of gastrointestinal bleeding during anticoagulant treatment
GI bleeding varies by type of NSAID and dosage, with slow-release formulations being the most likely to damage the mucosal lining. 11 Whenever possible, NSAIDs should be
Discussions should outline the risks of bleeding that come with resuming anticoagulation, including clinical signs of bleeding (e.g., monitoring for melena after GI bleeding), as well as implications for thrombotic events and death
In patients on oral anticoagulant and PPI co-therapy, NOACs were associated with lower risk of upper gastrointestinal bleeding and mortality compared to warfarin, while there was no
Gastrointestinal bleeding (GIB) is a potentially fatal and avoidable medical condition that poses a burden on global health care costs. The rate of major GIB related to the use of
Upper gastrointestinal (GI) bleeding is defined as hemorrhage from the mouth to the ligament of Treitz. Common risk factors for upper GI bleeding include prior upper GI
In 13,819 patients with moderate- and high-risk ACS randomized to receive bivalirudin (or heparin) plus a glycoprotein IIb/IIIa inhibitor, or bivalirudin monotherapy (ACUITY
Oral Anticoagulant and Proton Pump Inhibitor Cotherapy and GI Bleeding
The risk of major upper gastrointestinal tract bleeding, a frequent and potentially serious complication of oral anticoagulant treatment, 1,2 could be affected by the specific
Background Guidelines provide various recommendations for the use of proton pump inhibitors (PPI) to prevent upper gastrointestinal (UGI) bleeding in acute myocardial
Ray and colleagues 42 reported that PPIs decreased the risk of upper GI bleeding in patients on clopidogrel by 50% and decreased the risk of GI bleeding by 2.8% per year in patients with
However, these drugs have been associated with an increased risk of gastrointestinal (GI) bleeding. We conducted a systematic review and meta-analysis to
Most anti-inflammatory drugs have been associated with an increased risk of serious upper gastrointestinal complications. Epidemiological studies have estimated the

Conclusion: In patients on oral anticoagulant and PPI co-therapy, NOACs were associated with lower risk of upper gastrointestinal bleeding and mortality compared to
In patients on oral anticoagulant and PPI co-therapy, NOACs were associated with lower risk of upper gastrointestinal bleeding and mortality compared to warfarin, while there was no difference among the oral
However, it raises the risk of bleeding in the upper gastrointestinal tract (UGIB). The risk significantly increases if two antiplatelet agents are used, and it becomes even greater
Reduction of Upper Gastrointestinal Bleeding Risk With Proton Pump Inhibitor Therapy in Asian Patients With Atrial Fibrillation Receiving Direct Oral Anticoagulant: A
The type of bleeding lesion seen on endoscopy determines the risk of re-bleeding. This can assist with patient disposition, for example: Visible vessel: higher risk of re-bleeding.
Common risk factors for gastrointestinal bleeding (GIB) are advanced age and the use of antiplatelet or anticoagulants drugs for the prevention of cardiovascular diseases.
Among 1,643,123 patients taking oral anticoagulants, over 651,427 patient-years of follow-up, the adjusted incidence of hospitalization for upper GI bleed was 115/10,000 person-years (95%
Purpose of Review Gastrointestinal (GI) bleeding can carry minimal or significant risk for recurrent hemorrhage. Timing of feeding after GI bleeding remains an area of debate,
Background: To investigate risks of hospitalization for upper gastrointestinal bleeding (UGIB) in H. pylori-eradicated patients newly started on warfarin or direct oral anti-coagulants (DOACs).
Peptic ulcer bleeding is the most common cause for UGIB despite Helicobacter pylori (H Pylori) eradication treatment and proton pump inhibitor use. 1 While incidence of UGIB has been
Conclusion: CCI and duodenal bleeding are risk factors for re-bleeding in patients with NVUGIB who were receiving OACs, while low index albumin levels and previous PU and UGIB history
Gastrointestinal (GI) bleeding is the most frequent single site of oral anticoagulant (OAC)‐associated major bleeding. Patients with major GI bleeding experience morbidity and a
- Lineare Gleichungssysteme Schnittgerade
- Rumeurs Transphobes: La Justice Annule Une Procédure Intentée
- 10 Gold Reserviert Schilder Gastronomie
- Borgmann Media Verlag _ Borgmann Verlag Modernes Lernen
- Wetter Vias: 16 Tage Trend | Wetter Vias Frankreich 14 Tage
- Aktuelle Öffnungszeiten Des Sunpoint Sonnefeld
- Which Yoke Should I Get? – Best Yokes For Flight Simulator
- Stemming: Advantages And Limitations
- Ekg Kästner Anmeldung – Erich Kästner Oberstufe Anmeldung
- Kindertheater München Schauburg Programm
- Ferro Sulfide Latest Price, 0-5Mm Iron Pyrite Supplier, Exporter From China
- Je Souhaite Connaître Mon Numéro Client
- Zähne Auf Natur Reparieren: Natürliche Zähne Heilen
- Karten Für Trauzeugen
- Blutdruck Normalwerte: Alles In Einer Blutdrucktabelle